AION, Anterior optic neuropathy is an infarct of the cribrotic portion of the optic nerve, is manifested by a decrease in visual acuity in an abrupt and painless way, It may be transitory or not, depending on the cause that originates and the degree of involvement of the optic nerve.
There are two distinct types, well differentiated
1.-NON ARTERITIC AION.
It is the most frequent and least aggressive, with less visual difficulty than in the second type. It occurs in people between 45 and 65 years of age with a history of cardiovascular risk such as hypertension, Diabetes Mellitus, or the use of Viagra and hypercholesterolemia among others. The decrease in visual acuity is unilateral and painless. Losses of central, lateral or altitudinal vision usually appear when performing the visual field, being this a necessary test for its diagnosis.
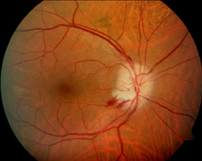
With the pupil dilated, exploring the fundus of the eye, on many occasions there are inflammatory signs or thickening of the nerve fibers of the optic nerve (edema), and linear hemorrhages around it or splinter hemorrhages.
It is essential to have treatment for all the factors that develop it, as well as the realization of an OCT(Optical Coherence Tomography) to see the degree of involvement of papillary edema and to be able to quantify it. Over time, this tends to be reduced, although a permanent alteration in vision in the area of the affected nerve may persist.
2.-ARTERITIC AION.
This is much more aggressive than the first and occurs in patients older than 70 years.The most common cause is giant cell arteritis. It is manifested by a sudden, painful and severe loss of visual acuity, fatigue, fever, headache, jaw claudication and paresthesias feeling in the temple área. All these symptoms and the appearance of the fundus, make the ophthalmologist suspect the process and prescribe an angiofluoresceingraphy for the correct diagnosis. Also a biopsy of the temporal artery (which is inflamed), and a blood test in which the factors that indicate inflammation, such as ESR and C-reactive protein are usually elevated.
The fundoscopic appearance is usually more variegated with a greater inflammation of the optic nerve as well as a greater number of retinal hemorrhages The natural evolution of this disease, ends in atrophy of the optic nerve. It is really a true ophthalmological emergency, being very important the early diagnosis and its treatment.

Recent Comments